The waiting room was full, but quiet in that tense way where people pretend to scroll on their phones while listening to every word through the door. A man in his forties walked out of the hepatologist’s office, looking stunned, staring at a leaflet like it was written in another language. A few minutes later, a woman in leggings and a work hoodie came out too, eyes glossy, repeating to herself: “But I don’t even drink.”
We’ve all been there, that moment when a doctor says something that doesn’t match the story we tell ourselves about our health.
Fatty liver disease sits right at the center of that mismatch. It doesn’t always hurt. It doesn’t scream. It just settles in quietly while life goes on, emails, kids, late dinners, glass of wine, maybe two.
The hepatologist I met that day said one thing that stuck with me.
People don’t just miss the signs — they often deny them.
“I Feel Mostly Fine”: The Silent Progression Nobody Wants to Hear About
The first thing this specialist pointed out was almost absurd in its simplicity: most people with fatty liver disease say they “feel fine.” Then they add, “just a bit tired, but that’s life, right?” That vague, dragging fatigue is one of the six signs she worries about most, because it gets brushed off as stress, age, or not sleeping enough.
She described patients who push through their days on coffee and willpower, thinking exhaustion is just the price of being busy. The liver is overloaded with fat, working overtime in the background. Yet on the surface, it looks like normal modern life.
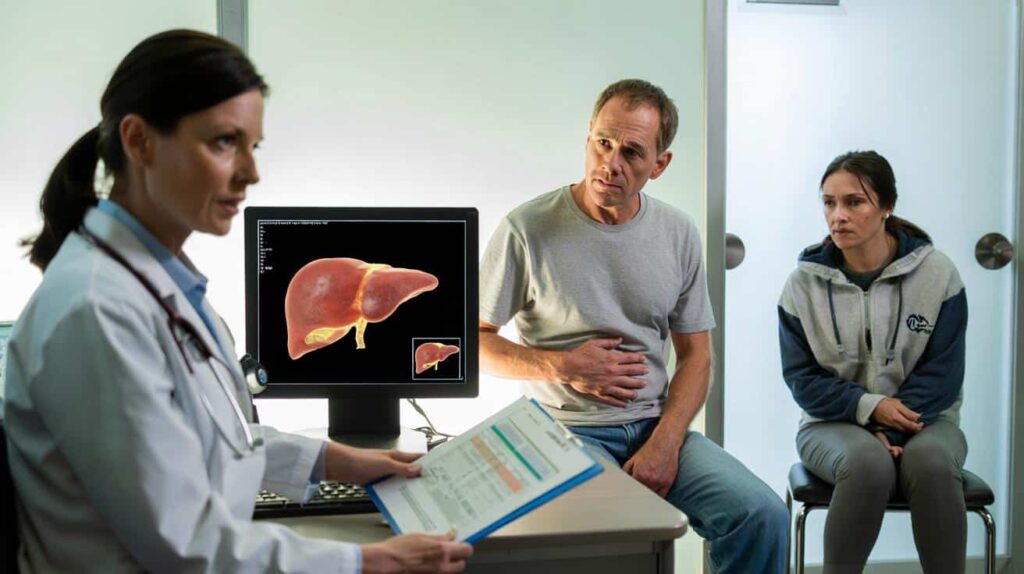
She told me about a 38‑year‑old delivery driver, father of two, who came in for routine blood tests needed for his job. Elevated liver enzymes. Ultrasound. Diagnosis: non-alcoholic fatty liver disease, already edging toward inflammation.
He had no sharp pain, no dramatic symptoms. Just constant tiredness, some brain fog, and a stubborn belly he joked about as his “dad tank.” He laughed when the doctor first mentioned his liver, then stopped laughing when she showed him the images.
The same pattern repeats with women in their thirties and forties, who blame their lack of energy on kids, night shifts, or hormones. The story sounds different, but the lab results look eerily similar.
Here’s the plain truth: our culture normalizes being exhausted, bloated, and slightly unwell.
The hepatologist explained that fatty liver disease builds quietly as fat infiltrates the liver cells. At first, the organ still copes. It’s a resilient filter, regenerating more than most organs can. Over time, though, excess fat triggers inflammation, then scarring. That’s when things stop being reversible so easily.
Those “mild” signs — fatigue, heavy digestion after meals, pressure under the right rib, unexplained weight gain around the waist — are like the fire alarm on low volume. Not a siren yet, but definitely not silence.
The 6 Overlooked Signs People Swear Are “Nothing Serious”
When we got into the details, the doctor listed the same six red flags she sees people minimize again and again. First: chronic fatigue that doesn’t match your actual workload. Second: a feeling of heaviness or slight pressure on the right side of the upper abdomen, especially after eating. Third: unexplained belly weight, even if the scale doesn’t move much.
The fourth sign surprised me: recurring nausea or a subtle loss of appetite on some days, followed by intense cravings on others. Fifth: changes in blood tests — abnormal liver enzymes that people ignore because “I feel okay.” And sixth: a kind of dull brain fog, trouble concentrating, forgetting simple things more than usual.
She told me about a teacher who had been living with four of those signs for years. She thought her abdominal discomfort was just gas, her brain fog was “end-of-term burnout,” and her lab results were “a bit off, but nothing dramatic,” as her GP had once put it.
 You don't need a mat — this 10-minute standing mobility routine is the secret to a stronger back
You don't need a mat — this 10-minute standing mobility routine is the secret to a stronger back
When she finally saw the hepatologist, her ultrasound showed clear signs of inflammation. Early-stage steatohepatitis — the phase where fatty liver shifts from being a silent guest to a destructive one. The teacher’s reaction? “I thought cirrhosis was only for alcoholics.”
That sentence still echoes in many consultation rooms. Non-alcoholic fatty liver disease now affects millions of people who barely drink, or who drink only on weekends and feel “reasonable” about it.
The logic behind these six signs is brutally simple. The liver is at the crossroads of metabolism: fats, sugars, toxins, hormones. When it’s overloaded with fat, its ability to filter, regulate, and store energy gets compromised. Fatigue is the body’s way of saying the system is operating on emergency mode.
Abdominal pressure stems from the liver swelling slightly or from changes in surrounding tissues. Brain fog often reflects metabolic imbalances that affect the brain as much as the liver. The sneaky part is that each sign taken alone looks banal. Put together, they paint a much darker picture.
*This is why the hepatologist keeps repeating the same sentence: “One sign might be coincidence. Two or three together deserve a check-up.”*
What a Hepatologist Wishes You’d Do at the Very First Doubt
When I asked her what she wished people would do earlier, her answer was disarmingly practical. Not a miracle detox. Not some exotic supplement. Just a simple, grounded sequence.
First, listen to your tiredness instead of romanticizing it as productivity. Second, write down your recurring symptoms for two weeks — fatigue level, digestion, discomfort, cravings, mood. Third, book a blood test that includes liver enzymes and talk about your notes with a professional.
“People show up so late,” she said, “because they wait for pain, and fatty liver doesn’t always play by the pain rule.”
She admitted she understands the denial. Nobody wants to be told their lifestyle is harming an organ they can’t even feel most days. Many of her patients are ashamed, convinced they “failed” at health, especially when weight or alcohol get mentioned.
She tries to dismantle that shame straight away. Fatty liver is strongly linked to genetics, sleep, stress, ultra-processed foods, sedentary jobs — things that don’t make you a bad person, just a human living in 2026. The mistake is not the condition itself. The mistake is deciding it’s not worth checking because “everyone is tired” or “my belly has always been like that.”
“People tell me, ‘I don’t want to know, it will stress me out,’” the hepatologist said quietly. “But the stress of not knowing while the disease progresses is far worse than the stress of catching it early, when we still have a lot of power to reverse it.”
- Listen to patterns rather than isolated days of fatigue or discomfort.
- Ask your doctor directly about your liver when you do routine blood tests.
- Don’t minimize abnormal liver enzymes, even if you feel relatively okay.
- Look at your waistline as a health signal, not just a clothing problem.
- Talk honestly about alcohol, even if your consumption seems “moderate.”
A Quiet Organ, Loud Consequences
The irony with fatty liver disease is that the organ at the center of the story never gets a voice. The heart can race, the lungs can burn, the stomach can cramp. The liver mostly stays silent until the damage is deep. That’s why these six subtle signs matter so much — they’re like whispers through a closed door.
Once fibrosis sets in, the road can bend toward cirrhosis, liver cancer, or transplant lists. That’s the part nobody wants to picture, yet it’s exactly what pushes some former deniers into radical, life-saving changes. And those changes, when started early enough, really can turn the story around.
| Key point | Detail | Value for the reader |
|---|---|---|
| Recognize the 6 subtle signs | Fatigue, right-side heaviness, belly weight, nausea/cravings, abnormal labs, brain fog | Helps you spot potential fatty liver disease before serious damage |
| Act on doubt, not on pain | Track symptoms, request liver tests, discuss results clearly with a doctor | Gives you a chance to reverse or slow progression while it’s still possible |
| Drop the denial narrative | Understand this isn’t just an “alcoholic’s disease” or a “lazy” problem | Reduces shame and motivates realistic, compassionate lifestyle changes |
FAQ:
- Question 1Can fatty liver disease really be reversed once detected?
- Question 2Do I need to drink alcohol to develop fatty liver problems?
- Question 3What tests should I ask for if I suspect fatty liver disease?
- Question 4Can skinny people still have fatty liver disease?
- Question 5How long does it usually take for lifestyle changes to improve the liver?



